- India
- International
Design of a new health system could emerge from the Covid crucible, for universal health coverage
Decentralised planning, delivery and monitoring are needed at the district level, with the district collector and the district health officer mobilising resources and coordinating operations.
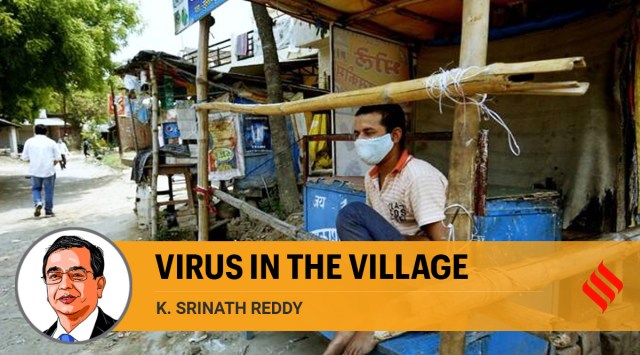 Man wearing a mask in Rae Bareli (Express Photo by Praveen Khanna)
Man wearing a mask in Rae Bareli (Express Photo by Praveen Khanna)The big cities battered by Covid-19 are now showing early signs of recovery from the second wave. There is growing concern now about smaller towns and rural areas where the virus has made inroads. Rising rates of transmission are superimposed on health systems that have been weak for long and essential health services have not been readily available or reliably efficient.
This is not true, of course, for all of India. States like Kerala and Tamil Nadu have strong health systems that reach remote rural areas. Even there, areas of tribal concentration are vulnerable. Many states in central and northern India have frail health systems which are especially feeble in rural areas. Infrastructure, health workforce, availability of drugs and other medical supplies, population health literacy and connectivity to higher levels of care are deficient in many districts.
During the first wave, the virus did not have easy passage into rural areas. Travel restrictions, prescribed or voluntary, prevailed even after the lockdown was lifted. Large gatherings were mostly avoided. Even where the virus entered, it had slow transmission as villages have lower population density than urban areas — people live in relatively ventilated houses and work in open fields. Because co-morbidities like hypertension, diabetes and cardiovascular disease are lower in rural populations, risk of severe illness and death was also less. Rural health services were not severely challenged during the first wave, except in districts where urban-rural connectivity was high and differences in development were narrow.
However, the events leading to the second wave saw a change of script. Elections saw vigorous campaigning, huge crowds and frequent visits by outsiders. The Kumbh Mela and regional festivals saw many villagers travel and return with the virus. This time, it was not just the wild virus but also the more infectious variants. Erroneously assumed countrywide herd immunity and lack of anticipation of the second wave became the Trojan horses by which the virus evaded rural defences.
We now need to respond vigorously to contain the threat and limit the damage. The Standard Operating Procedures released by the Ministry of Health and Family Welfare on May 16 for “Covid-19 Containment & Management in Peri-urban, Rural & Tribal areas” are well-framed and timely. They cover surveillance, screening, isolation and referral; home and community-based isolation; monitoring of active cases in home isolation; health infrastructure (such as Covid Care Centre at sub-centre or PHC level and a Dedicated Covid Health Centre at CHC or sub-district level); trained human resources; in-patient and out-patient services; clinical management; home care; post-Covid management; community mobilisation; risk and behaviour change communication.

The proposed protocols are good in most parts but some areas will need a fresh look or modification. Household visits by frontline health workers for surveillance of Covid symptoms is to be followed by Rapid Antigen Test (RAT) of any suspected case. While RAT is easier to use than RT-PCR, it has a higher rate of false negative results. Either repeat tests have to be done after a few days in such cases or a composite clinical diagnosis has to drive the decisions for isolation and case management.
Recommended drugs include hydroxychloroquine (which has shown no benefit for prevention or treatment in large clinical trials) and ivermectin (of uncertain benefit as yet, with WHO cautioning that use should be restricted to clinical trials). Many states may prefer to develop their own treatment protocols which have greater scientific strength.
While primary healthcare teams must indeed conduct household visits for symptom surveillance and case detection, timely testing, triage and referral as needed, home care support and monitoring, they are likely to be hard-pressed with multiple duties. Engagement of the local community is vital. Where available, NSS and NCC resources can be drawn upon. Community-based organisations, which have grassroots presence, can assist in the delivery of health and social services.
Emergency transport systems that can transfer seriously ill patients to pre-determined points of advanced care and mobile laboratories must be organised with assurance of availability, affordability and equity. Other than for essential needs, commuting between urban and rural areas must be restricted to reduce the risk of transmission. Large gatherings must be prohibited for at least six months.
Vaccine delivery would depend on availability, which seems constrained at present. Those aged above 45 years and younger persons with co-morbidities must be given priority in vaccination. As the access to and familiarity with smartphones will be limited, primary healthcare teams and citizen volunteers should assist age-eligible persons for registration. Since many persons may be unaware of their blood pressure or blood sugar values, all persons above 30 years of age may be offered screening of blood pressure and blood sugar at the health sub-centre or a convenient location in the village. Point-of-care diagnostic devices can be supplied for this purpose. Technology-enabled frontline health workers can catalyse the transformation of healthcare, as we configure health systems for the future.
The vaccination drive can serve to advance screening and counselling for hypertension and diabetes. These are integral to the template of comprehensive primary care proposed in the National Health Policy, 2017. Other health programmes too must be attended to through engagement of communities and NGOs. Supportive social services can be extended through such partnerships.
Decentralised planning, delivery and monitoring are needed at the district level, with the district collector and the district health officer mobilising resources and coordinating operations. While support from the police will be essential, public health should not be viewed as a law enforcement issue. Decentralised, data-driven decision making must be enabled by easily operable and reliable information systems. Essential data must be readily available locally at the block level for real-time alerts and rapid response. Expanded data sets can be analysed at the district level for monitoring and supportive supervision. More elaborate (optimal) data sets can flow to the state capital level for course corrections and resource allocation. At the local level, qualitative information from key informant interviews must supplement quantitative data to help in identifying roadblocks and solutions.
Perhaps the design of a new health system will emerge from the Covid crucible to serve as the platform for universal health coverage.
This column first appeared in the print edition on May 18, 2021 under the title ‘Virus in the village’. The writer, a cardiologist and epidemiologist, is President, Public Health Foundation of India
EXPRESS OPINION
More Explained
Apr 27: Latest News
- 01
- 02
- 03
- 04
- 05